
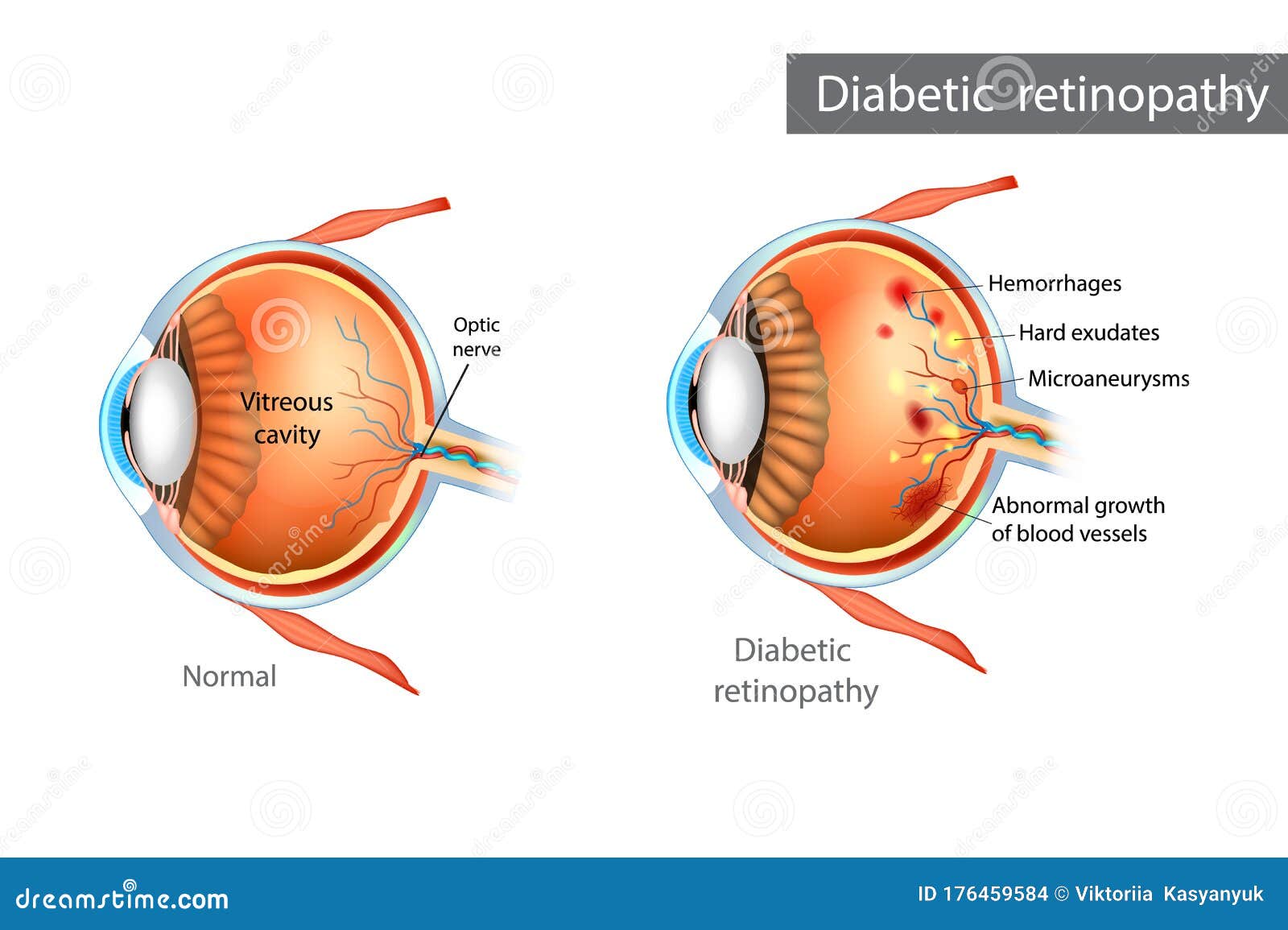
They will take photographs of the eye’s interior to look for the presence of: These drops dilate the pupils and allow the doctor to view the inside of the eye. The following methods can help eye doctors diagnose diabetic retinopathy: Dilated eye examįor a dilated eye exam, an eye doctor places drops into the person’s eyes. It is important that people with diabetes have an eye examination at least once a year or when a doctor recommends that they do. However, an eye specialist, called an ophthalmologist, can detect the signs. The blockage causes a buildup of pressure in the eye, increasing the risk of optic nerve damage and vision loss.ĭiabetic retinopathy generally starts without any noticeable change in the vision. The normal flow of fluid in the eye may become blocked as new blood vessels form, leading to glaucoma. A detached retina presents a significant risk of total vision loss if a person does not get treatment. It usually causes the appearance of floating spots in the individual’s field of vision, flashes of light, and severe vision loss. This complication can happen if scar tissue pulls the retina away from the back of the eye. In some cases, diabetic retinopathy can lead to a detached retina. If the retina remains undamaged, bleeding in the vitreous can resolve itself. In mild cases, the symptoms include floaters, but more severe cases can involve vision loss, as the blood in the vitreous blocks light from entering the eye. When blood vessels bleed into the main jelly that fills the eye, known as the vitreous, this is called vitreous hemorrhage. Without treatment, diabetic retinopathy can lead to various complications. More than 2 in 5 people with diabetes in the United States have some stage of diabetic retinopathy.ĭiabetes also increases a person’s risk of developing other eye problems, including cataracts and open-angle glaucoma. Once a person gets their blood sugar levels under control, the lens will usually return to its original shape, and vision will improve. This fluid accumulation changes the shape and curve of the lens, causing changes in vision. The eye may accumulate fluid during long periods of high blood sugar. The early stage is known as nonproliferative diabetic retinopathy. If the eye starts to grow new blood vessels, this is known as proliferative diabetic retinopathy, which experts consider a more advanced stage. The eye may then grow new blood vessels that are weaker and leak or bleed more easily. If sugar blocks the tiny blood vessels that go into the retina, it can cause them to leak or bleed.

It detects light and sends signals to the brain through the optic nerve. The retina is the membrane covering the back of the eye. Over time, having too much sugar in the blood can damage blood vessels throughout the body, including in the retina. It can arise as a result of the high blood sugar levels that diabetes causes. Diabetic retinopathy is an eye condition that occurs due to diabetes.


 0 kommentar(er)
0 kommentar(er)
